Contents
Homeostasis
Importance of Homeostasis
Homeostasis is the maintenance of a constant internal environment via physiological control systems. These control systems keep temperature, blood pH, blood glucose, and water potential within set limits.
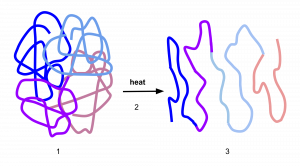
If body temperature is too low, there will be insufficient kinetic energy for enzyme-controlled reactions. If body temperature is too high, enzymes will denature. Either way, metabolic reactions could slow to the point that cells die. Alterations in blood pH will also result in enzyme denaturation.
Glucose is needed for respiration, so a lack of glucose in the blood could result in cell death. If blood glucose levels are too high, then this will lower the water potential of the blood and water will leave surrounding cells by osmosis, preventing normal cell function. If the water potential of the blood is too low, water will move into cells by osmosis and can cause them to burst.
Negative Feedback
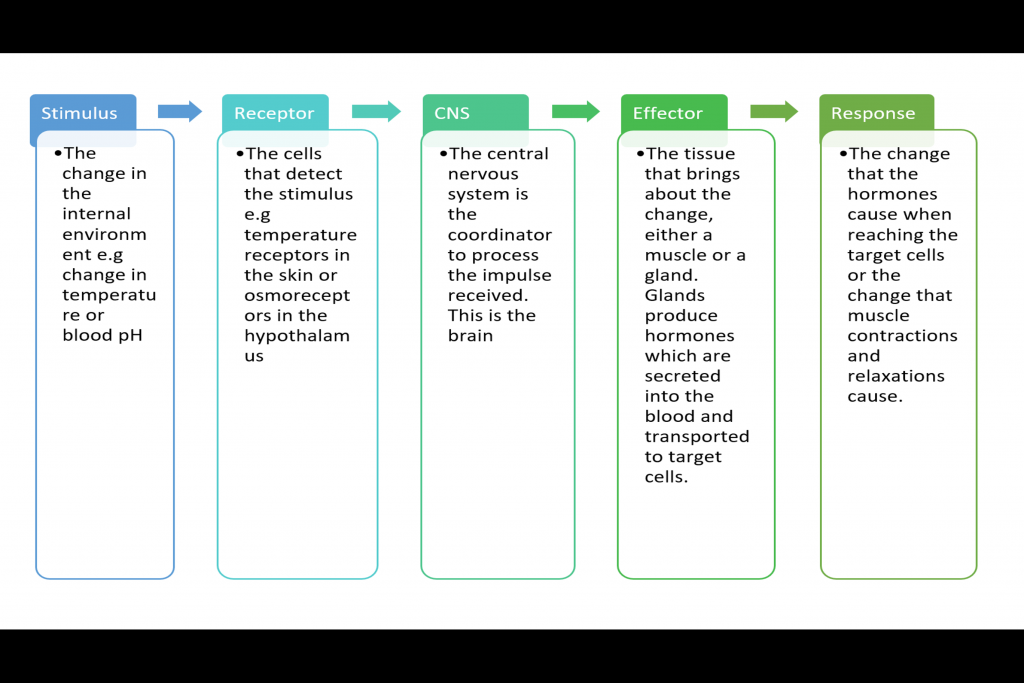
Negative feedback is how deviation from the normal values are restored systems to their original level. This involves the nervous system and often hormones too, as shown in the flow diagram:
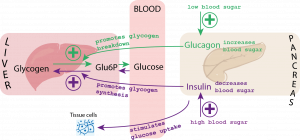
Blood Glucose Control
Blood glucose will increase following ingestion of food or drink containing carbohydrates and will fall following exercise or if you have not eaten.
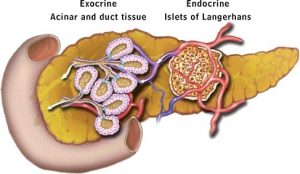
The pancreas detects changes in the blood glucose levels and contains endocrine cells in the Islets of Langerhans which release the hormones insulin and glucagon to bring blood glucose levels back to normal. Adrenaline is released by adrenal glands if your body anticipates danger and results in more glucose being released from stores of glycogen in the liver.
Key Terms:
- Glycogenesis (genesis means to make)
This is the process of when excess glucose is converted to glycogen in blood glucose is higher than normal. This occurs in the liver and the liver can store 75-100g of glycogen. This would last you 12 hours at rest if you do not eat.
- Glycogenolysis (lysis means to breakdown)
This is the breakdown of glycogen back into glucose in the liver. This occurs when blood glucose levels are lower than normal.
- Gluconeogenesis (Amino acids to glucose)
This is the process of creating glucose from non-carbohydrate stores in the liver. This will occur if all glycogen has already been hydrolyzed back into glucose and your body still needs more glucose. The above processes are controlled by the three hormones insulin, adrenaline, and glucagon.
The Action of Insulin Beta cells in the Islets of Langerhans detect if blood glucose is too high and will secrete insulin. Insulin will decrease blood glucose in the following ways:
- Attaching to receptors on the surfaces of target cells. This changes the tertiary structure of the channel proteins resulting in more glucose being absorbed by facilitated diffusion.
- More protein carriers are incorporated into cell membranes so that more glucose is absorbed from the blood into cells.
- Activating enzymes involved in the conversion of glucose to glycogen. This results in glycogenesis in the liver.
The Action of Glucagon
- Attaching to receptors on the surfaces of target cells. When glucagon binds, it causes a protein to be activated into adenylate cyclase and to convert ATP into a molecule called Cyclic AMP (cAMP). cAMP activates an enzyme, protein kinase, that can hydrolyze glycogen into glucose.
- Activating enzymes involved in the conversion of glycerol and amino acids into glucose.
The Role of Adrenaline
- Adrenaline attaches to receptors on the surfaces of target cells. This causes a protein (G protein) to be activated and to convert ATP into cAMP. cAMP activates an enzyme that can hydrolyze glycogen into glucose. This is known as the second messenger model of adrenaline and glucagon action because the process results in the formation of cAMP, which acts as a second messenger.
Diabetes
This is when blood glucose cannot be controlled.
Type I diabetes is due to the body being unable to produce insulin. It starts in childhood and could be the result of an autoimmune disease where the beta cells were attacked. Treatment involves injection of insulin.
Type II diabetes is due to receptors on the target cells losing their responsiveness to insulin. It usually develops in adults because of obesity and poor diet. It is controlled by regulating intake of carbohydrates, increasing exercise, and sometimes insulin injections.
Osmoregulation
This is the process of controlling the water potential of the blood.
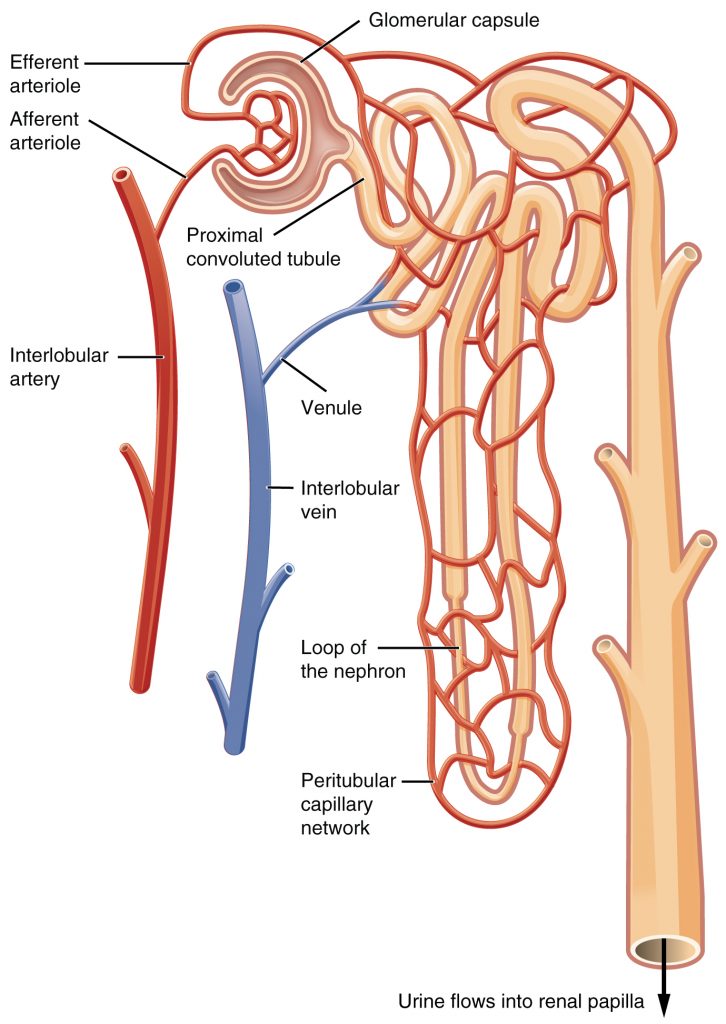
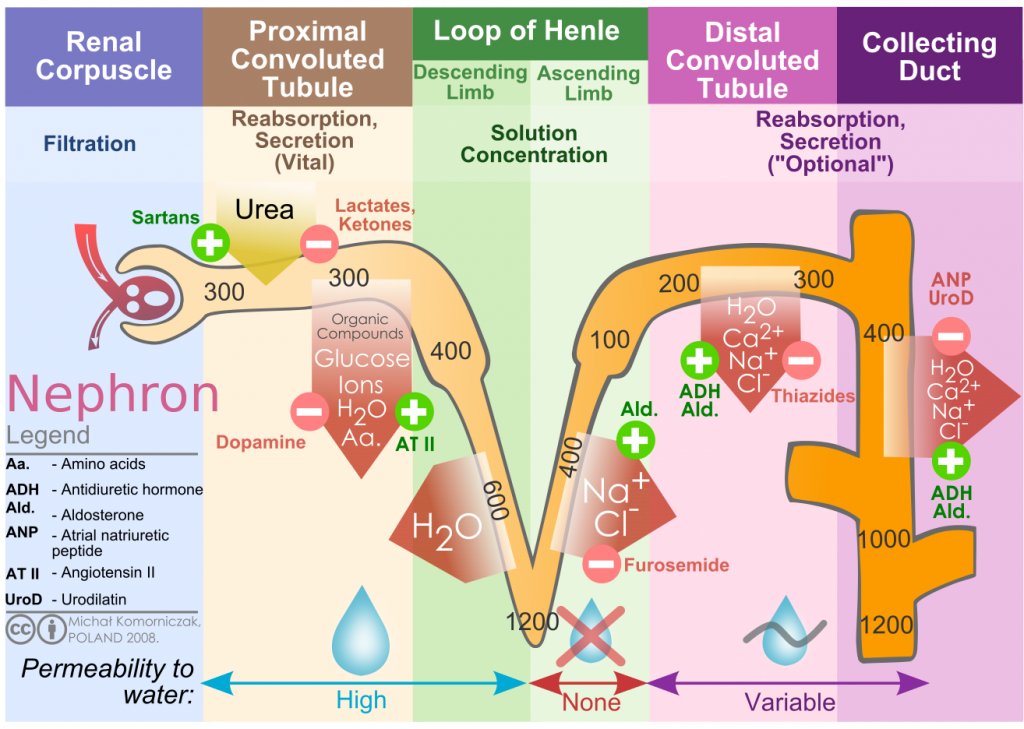
The nephron is a structure in the kidney where the blood is filtered, and useful substances are reabsorbed into the blood. This is shown in the diagram below.
Nephron Structure
- The Bowman's (renal) capsule - Ultrafiltration occurs here because the afferent arteriole (entering the glomerulus) is wider than the efferent arteriole (leaving the glomerulus), creating high hydrostatic pressure. Small molecules and water are forced out of the capillaries into the renal capsule, and large proteins and blood cells remain in the blood.
- Proximal convoluted tubule - The walls are made of microvilli epithelial cells to provide a large surface area for diffusion of glucose into the cells from the PCT. Glucose is then actively transported out of the cells into the intercellular space to create a concentration gradient. Glucose can then diffuse into the blood again.
- Loop of Henle - Sodium ions are actively transported out of the ascending limb into the medulla to create a low water potential. Water moves out of the descending limb and out of the distal convoluted tubule and collecting duct by osmosis due to this water potential gradient.
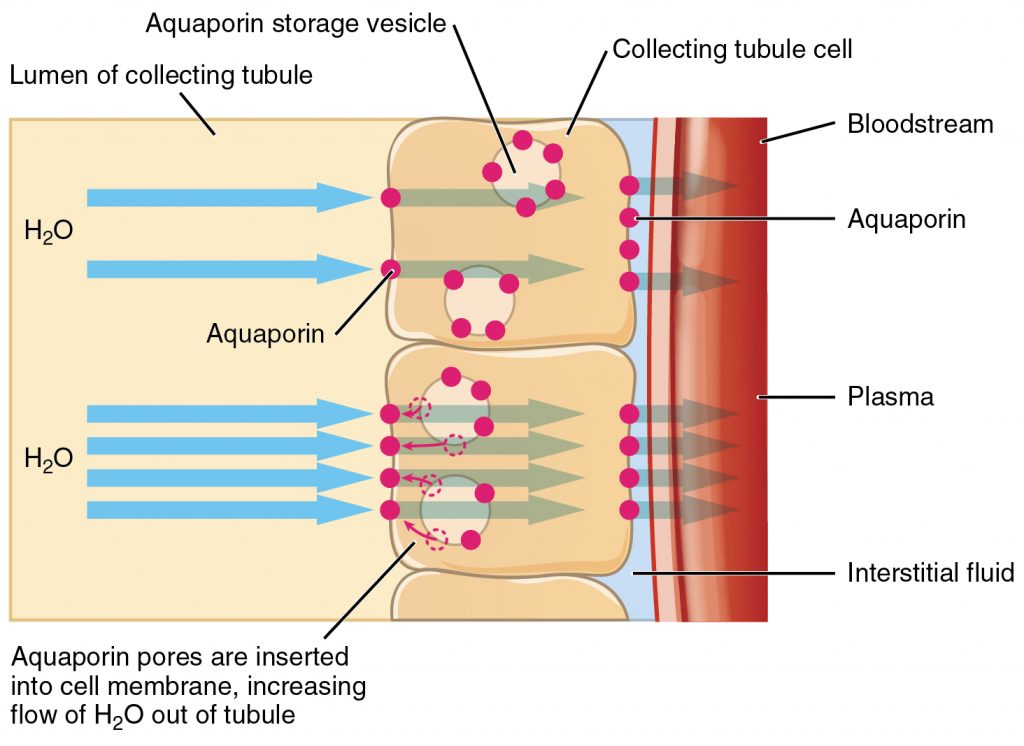
The liquid remaining in the collecting duct forms the urine. It contains water, dissolved salts, urea, and other substances such as hormones. More or less water can be reabsorbed at the collecting duct depending on the water potential of the blood. The hypothalamus in the brain monitors the water potential of the blood. If the water potential of the blood decreases, water will move out of the osmoreceptor cells by osmosis, resulting in the cells shriveling. This triggers other cells in the hypothalamus, which send a signal to the posterior pituitary gland. The posterior pituitary will then release antidiuretic hormone (ADH) into the blood.
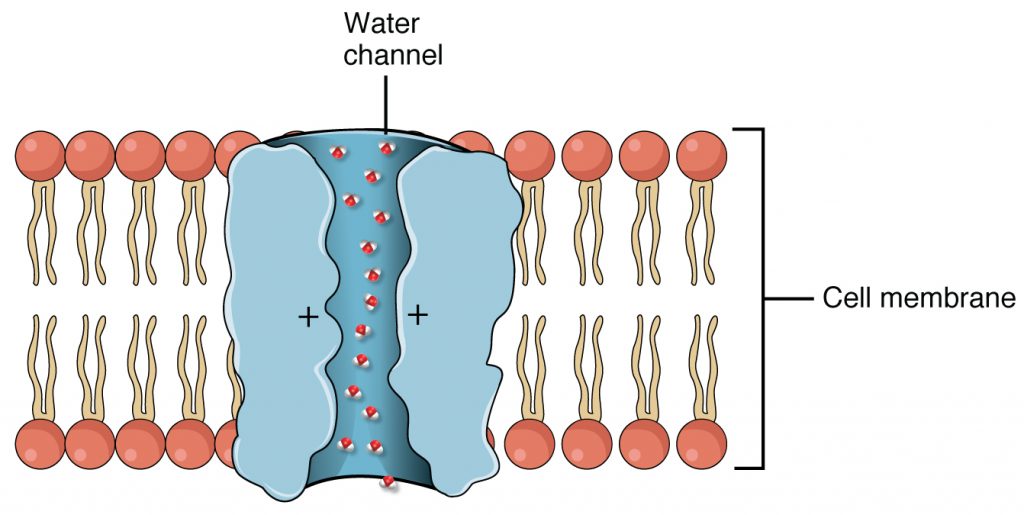
ADH will bind to complementary receptors that are only located on target cells in the DCT and collecting duct. When it binds, it activates adenyl cyclase to make cAMP. This activates an enzyme that causes vesicles containing aquaporins to fuse with the membrane. Aquaporins are channel proteins that allow water to transport across the membrane. As a result, the membrane becomes more permeable to water and more will leave to be reabsorbed back into the blood.
- Why do hormones only affect their target cells and not other cells?
- Your answer should include: cell / surface / membrane
- What are the hormone-producing cells called inside of the pancreas?
- Your answer should include: Islets / of / Langerhans
- Why is it harmful if there is too much glucose in the blood?
- Your answer should include: reduces / water / potential
- Why is it harmful if there is not enough glucose in the blood?
- Your answer should include: glucose / respiration
- Where is ADH released from?
- Your answer should include: pituitary / gland
- What does ADH stand for?
- Your answer should include: anti-diuretic / hormone
- What effect does ADH have on the collecting duct?
- Your answer should include: permeable / water